
A recent survey found that the average wait time for a new patient to see a physician in 15 of the largest cities in the U.S. was 26 days, up from 24.1 days in 2017. Timely access to health care providers has long been an issue, but appears to be worsening in certain geographies and provider types. Until recently, timely access to care was regulated at the state level; however, in April, the Centers for Medicare & Medicaid Services (CMS) unveiled its proposed rule to address the issue. The Notice of Proposed Rulemaking Managed Care Access, Finance, and Quality (CMS-2439-P) (NPRM) only applies to enrollees in Medicaid and Children’s Health Insurance Program (CHIP), which together cover more than 90 million beneficiaries across the U.S. While both programs offer fee-for-service and managed care plans, more than 70 percent of beneficiaries enroll in managed care plans.
Routine Appointments
The NPRM proposes a national maximum standard for appointment times for routine appointments for primary care (adult and pediatric) and outpatient mental health and substance use disorder (MHSUD) (adult and pediatric). It also proposes an appointment time standard for obstetric/gynecological (OB/GYN) services as well as a “state-selected service” (adult and pediatric, if appropriate). The “state-selected service” is to be chosen by the state in a provider type that addresses access issues specific to that state.
Under the proposed rulemaking, as long as states stay within CMS’s ceiling standard, they have flexibility to develop appointment wait time standards that reflect the needs of their Medicaid and CHIP managed care populations, as well as local provider availability. Each state’s maximum appointment waiting time cannot be more than 10 business days for routine outpatient MHSUD appointments and not more than 15 business days for routine primary care (adult and pediatric) and OB/GYN appointments. CMS did not propose a maximum time for the state-selected service, but requires each state to establish its own time frame in an evidence-based manner.
Appointment Waiting Time Standards
The proposal also allows the states to vary appointment wait time standards for the same provider type, for example, by adult versus pediatric patients, telehealth versus in-person, geography or service type, etc.
Additionally, just as CMS did not propose a maximum appointment waiting time for the state-selected service, the agency also chose not to propose a maximum wait time for non-urgent specialist appointments. In so doing, CMS stated it believed that Medicaid managed care standards should focus on primary care, OB/GYN and MHSUD. For the time being, CMS also chose not to provide appointment time standards for urgent and emergent care.
State Monitoring and Reporting
The NPRM calls for each state’s Medicaid agency to monitor the appointment wait times of its contracted managed care plans through an independent entity. The independent entity is expected to conduct “secret shopper” surveys using a statistically valid, randomized sample of providers to determine compliance. If a managed care plan’s results are non-compliant, detailed corrective action plans are proposed. Survey results may report, as a separate number, appointment wait times for telehealth visits only if providers also offer in-person appointments to enrollees.
Furthermore, the NPRM requires states to conduct an annual enrollee experience survey of each Medicaid managed care plan, for which results must be posted on the plan’s website and reported to CMS.
Other Requirements
The proposed rule also seeks to make double use of the “secret shopper” surveys by identifying errors in plan’s provider networks for the above categories (e.g., primary care and OB/GYN). CMS believes that these survey results can be useful information for plans and that the data will shed light on how often network providers are providing routine appointments that abide by state standards and whether states' networks actually have capacity to serve the number of enrollees expected in each service area. Ideally, CMS wants each state to collect four pieces of data for each electronic provider directory: the active network status with the plan, street address, telephone number and whether the provider is accepting new enrollees. Survey results, including provider directory errors, should be reported to CMS on an annual basis. Furthermore, states must also submit an annual payment analysis comparing managed care plan payment rates for certain services as a proportion of Medicare’s payment rate.
The proposed compliance deadline is 3 years after the final rule’s effective date.
Finally, the Medicaid agencies must compile all of the aforementioned information on a single webpage that is easily accessible to the public.
Final Notes
The proposed rule has a public comment period open until July 3, 2023 and impacted managed care plans are highly encouraged to submit comments here regarding the feasibility and cost of both the requirements and the effective date. The final rule is expected to be published in 2024.
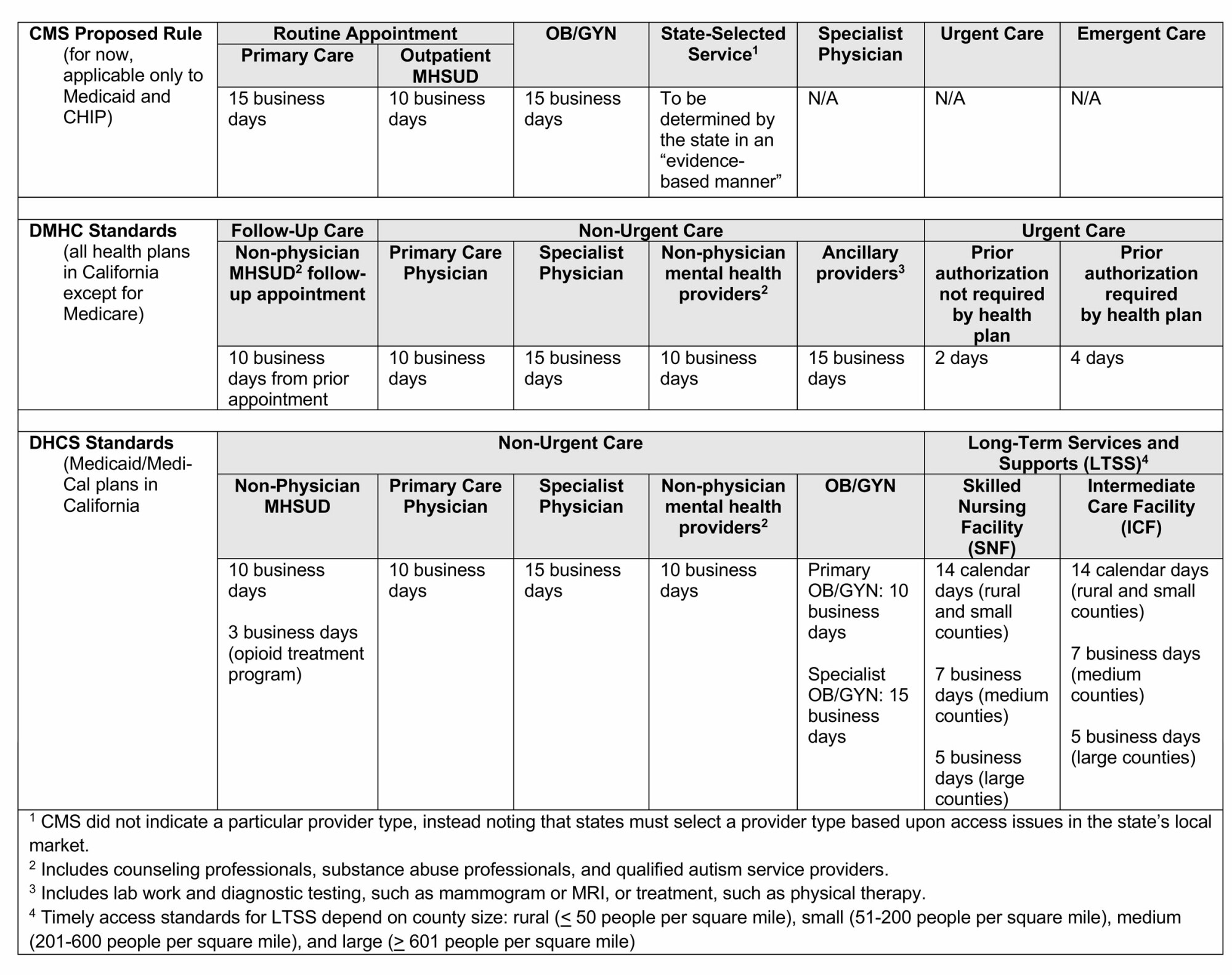
Managed care plans should also compare the CMS proposal against their existing state requirements. For example, California already has two sets of timely access requirements—one for commercial plans and another for Medi-Cal plans—see the comparison chart below. Plans with multiple lines of business especially may find compliance with the numerous, differing requirements difficult to track and administer. Thus, Nossaman strongly recommends written policies and procedures, appropriate employee and provider training, tracking and trending of access-related grievances, effective delegation oversight and corrective action plans and properly worded provider contracts.
Our Health Law Ticker is a one-stop resource for everything new and noteworthy medical staffs and peer review. We cover recent developments in healthcare legislation, litigation, regulatory compliance, HIPAA, peer review, medical staffs and general operations for healthcare delivery systems.
Stay Connected
 RSS Feed
RSS Feed
